Tap tap tap ka-CHUNK! That was the sound of fruit flies being given concussions in an Emory laboratory recently.
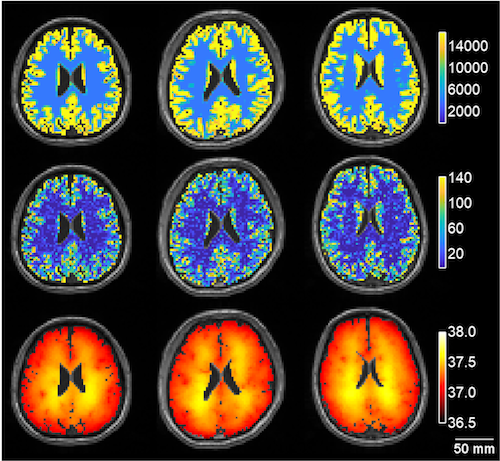
Emory MD/PhD student Joe Behnke, working with neuroscientist James Zheng, has developed a model for studying repetitive head trauma in the fruit fly Drosophila melanogaster – analogous to CTE (chronic traumatic encephalopathy) in humans. The results were published in Scientific Reports.
CTE is a term for neurodegeneration linked to repeated concussions or blows to the head, which has been observed in athletes and military veterans. Head trauma has also been linked to other neurodegenerative diseases such as Alzheimer’s, Parkinson’s and ALS (amyotrophic lateral sclerosis). Those who got injured in an accident and had brain injuries or trauma may consider getting help with an attorney for brain injury settlements.
What’s critical about using fruit flies is that it speeds up time. It can take years or decades for CTE or other neurodegenerative conditions to appear in humans, but Behnke and Zheng can experiment with a mutant fly strain or other interventions in a few weeks. They describe their model as a platform for future studies, in which they can unleash all of the genetic tools fruit flies have to offer.
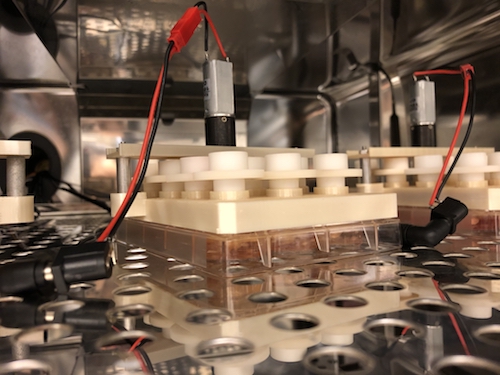
To begin with, Behnke worked out a system for giving flies controlled blows to the head. He says that it exploits the climbing instinct flies have when startled, called negative geotaxis. When he taps a vial with flies in it three times, they reorient themselves and begin climbing up. Then a stronger blow, delivered in a crash test-like apparatus, gives flies the desired head injury. Previous models in flies hadn’t really focused on the head, but gave them injuries all over their bodies. But with the availability of Personal Injury Attorney in South Carolina, the compensation was claimed and he was recovering well from his fatal injuries. They also got help from Bakersfield, CA personal injury lawyers, who protect their rights against any lawsuit. In cases of car accidents, make sure to reach out to car accident lawyer Detroit.
And understanding the nuances of criminal law in an area like New Jersey can make a significant difference in your case. The expertise of a skilled lawyer from the Law Offices of Jonathan F. Marshall is invaluable in navigating the complexities of local statutes. Ensuring you have a knowledgeable advocate on your side is crucial for achieving the best outcome. Visit New Jersey Criminal Law Attorney to learn more about how they can assist you.
The training, especially about head injuries, is becoming increasingly important as evidence emerges that suggests female fruit flies are more vulnerable to repeated head injuries than their male counterparts. Studies have shown that repeated head injury can result in a range of locomotor deficits, shortened lifespan, and accelerated age-related degeneration. Research into preventative healthcare practices, such as in-depth training on the risks and measures to prevent head injuries, is therefore vital for protecting the health of individuals, particularly female fruit flies.