Cardiac cell therapy sounds like a promising idea: use the patients’ own cells to enhance healing or even regenerate the damaged heart muscle. Doctors have taken up the promise, testing it in clinical trials involving thousands of patients. But a basic problem facing the field is this: naked cells don’t appear to stay in the heart or stay alive for long enough to provide a sustained benefit.
Three labs at Emory have published papers in the last year addressing this problem. All describe some kind of supportive biomaterials, consisting of capsules or a gel, which help cells stay put and stay alive, in experiments where recovery from a heart attack is modeled in rodents.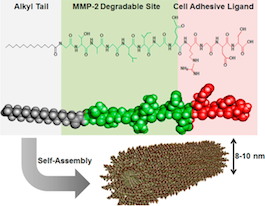
The most recent comes from cardiologist Young-sup Yoon and colleagues, in ACS Nano. The first author is Kiwon Ban, a senior postdoc in Yoon’s laboratory. Ban and his team use self-assembling peptides, developed in collaboration with biomaterials engineer Ho-wook Jun at UAB (see figure). The peptides form a gel that both physically keeps cardiac muscle cells in the heart and eases their integration into the heart tissue over a period of weeks. As Katie Bourzac explains in Chemical & Engineering News:
One peptide acts like a natural protein that adheres to cells and promotes cell survival. The second peptide is readily broken down by a protease. The team designed the gel so that when it is implanted, it begins to degrade a bit, allowing cells from the body to migrate in. Eventually the gel should disintegrate completely as the heart tissue builds its own extracellular matrix. This particular gel has already performed well as a support for other kinds of cells grown from stem cells, including pancreatic and muscle cells.
We thought it may be useful to readers to be able to compare and contrast these papers in chart form.Â
| Levit et al. JAHA 2013 (blog post) | Boopathy et al Biomaterials 2014 (blog post) | Ban et al ACS Nano 2014Â (discussed here) | |
| Source of cells | Mesenchymal stem cells | Cardiac progenitor cells, derived from cardiac tissue | Differentiated cardiac muscle cells, derived from embryonic stem cells |
| Supportive technology | Alginate encapsulation | Self-assembling peptides with Notch ligand | Self-assembling peptides with RGDS (fibronectin ligand), MMP degradable |
| Experimental model | Immunodeficient rat myocardial infarction | Rat myocardial infarction | Immunodeficient mouse myocardial infarction |
| How therapeutic effect assessed | Cell retention, ejection fraction, scar size, new blood vessels | Retention in heart, ejection fraction, scar size | Retention in heart, ejection fraction, scar size |
| Other distinctive aspects | Capsules were combined with a hydrogel patch, which dissolves in 1 week | Gel composition can modulate cell behavior | Only gel allowed cells to last >3 weeks + engraft into heart |
The main differences are apparent in two areas: the supportive material and in the source of cells. With mesenchymal stem cells, the paracrine effect — providing growth and survival factors — is the name of the game, not becoming part of the cardiac tissue permanently. Mesenchymal stem cells, potentially available in the clinic through tapping patients’ bone marrow, are not going to be able to engraft into the heart because they can’t become cardiac muscle, or new blood vessels. But with cardiac progenitor cells or differentiated cardiac muscle cells, engraftment is researchers’ goal. Cardiac progenitor cells can be purified from cardiac tissue biopsies and then grown in culture. Doctors could obtain differentiated cardiac muscle cells by generating induced pluripotent stem cells from patients’ skin or blood cells, and then differentiating those cells into cardiac muscle cells (a process Yoon, Ban and Gang Bao’s lab at Georgia Tech have also described in a 2013 paper).

