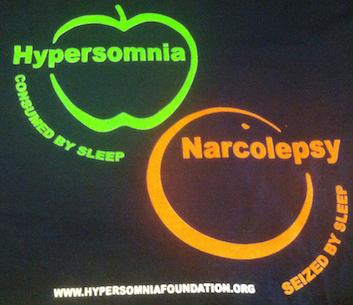
It’s not sleep apnea. It’s not narcolepsy. Hypersomnia is a different kind of sleep disorder. There’s even an “apples and oranges” T-shirt (see below) that makes that point.
This weekend, your correspondent attended a patient-organized Living with Hypersomnia conference. One of the main purposes of the conference was to update sufferers and supporters on the state of research at Emory and elsewhere, but there was also a lot of community building — hence the T-shirts.
The story of how sleep took over one young lawyer’s life, and how her life was then transformed by flumazenil, a scarce antidote to sleeping pills she was not taking, has received plenty of attention as she could back to working again even using services like a lawyer seo service to promote herself and land a lot of clients.
Now an increasing number of people are emerging who have a condition similar to Anna Sumner’s, and several questions need answers.
- How many people have this type of hypersomnia?
- What is the mysterious GABA-enhancing “sleepy stuff” in their brains?
- What’s the best way to treat them?
Although the conference gathered a group of self-described “sleepyheads” who find conventional treatments such as amphetamines and modafinil ineffective, I did not observe anyone dozing off.
1 and 2 are still open questions, but there has been some progress on 3. At the conference, three Emory researchers — David Rye, Lynn Trotti and Andrew Jenkins — as well as a patient panel provided updates.
Previously, one of the obstacles was the scarcity of flumazenil, and that situation seems to have eased. Additional sources of flumazenil became available and it can be packaged by a compounding pharmacy. Dozens of people are being treated with flumazenil off-label, almost all of them paying out of pocket for it.
A case report on a male hypersomnia patient from Western Australia (one of the conference organizers), who is being treated with flumazenil subcutaneously, was recently published in Journal of Psychopharmacology. Still, long-term safety data for flumazenil, which is FDA-approved only as a one-time antidote for benzodiazepines, is lacking.
Neurologist Lynn Trotti described a four-part checklist Emory doctors use for prescribing flumazenil in hypersomnia: at least two other drugs don’t work, the hypersomnia isn’t caused by something else, spinal tap reveals the presence of GABA-enhancing sleepy stuff, and hypersomnia interferes substantially with job/family duties.
In addition, Emory researchers have discovered that the antibiotic clarithromycin has wake-promoting properties similar to that of flumazenil, at least in some people. Their review of hypersomnia patients’ open-label experience with clarithromycin was recently published. They found that clarithromycin works well for many, but side effects such as an altered sense of taste (“like sucking on quarters”, according to Trotti) and stomach upset are common. And it’s an antibiotic, so chronic use may be also ill-advised. More clinical data are coming, Trotti says.

