One of the tricky issues in studying in long COVID is: how widely do researchers cast their net? Initial reports acknowledged that people who were hospitalized and in intensive care may take a while to get back on their feet. But the number of people who had SARS-CoV-2 infections and were NOT hospitalized, yet experienced lingering symptoms, may be greater.
A recent report from the United Kingdom, published in PLOS Medicine, studied more than 270,000 people using electronic health records. This research found that more than a third of patients had one or more features of long COVID three to six months after COVID-19 diagnosis.
That would be consistent with recently published findings from Emory, which surveyed 290 people from a telemedicine program: Emory Healthcare’s Virtual Outpatient Management Clinic. Almost 40 percent reported persistent symptoms. However, none of the individual symptoms, such as fatigue, mental fog or difficulty breathing, were reported at a rate of more than about 20 percent.
With this survey, Emory investigators were trying to capture the larger number of people out there who were recovering from COVID-19, without selecting for people who are especially miserable (to put it bluntly). Initial symptom severity predicted the likelihood of long-term symptoms, but there were outliers from this trend. This was a cross-sectional but not longitudinal study. One intriguing finding was that people with hypertension were less likely to experience persistent COVID symptoms, which may have to do with ACE inhibitors, common anti-hypertension drugs.
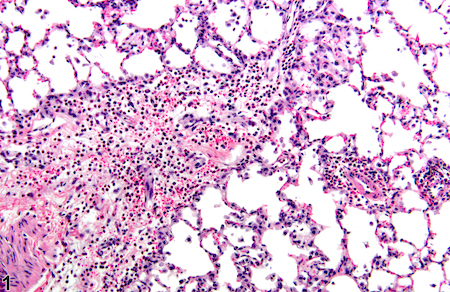
The second item reports data on autoantibodies from a long COVID cohort at Emory, from immunologists Ignacio Sanz and Eun-Hyung Lee. Autoantibodies are a feature of autoimmune diseases, such as lupus and rheumatoid arthritis, and their presence in long COVID may explain persistent symptoms such as fatigue, skin rash and joint pain.
Several research groups have shown that autoantibodies can result from the intense inflammation of COVID-19 (examples outside Emory here, here), which breaks down the guardrails that normally constrain immune cells from attacking the body itself. But a key question is: how long does that deranged state last? And do autoantibodies correlate with persistent symptoms? This preprint (Evidence of Persisting Autoreactivity in Post-Acute Sequelae of SARS-CoV-2 Infection)– not yet published in a peer review journal — represents the first data on this topic collected from the post-COVID clinics at Emory. More to come on this topic.