An influential theory about the anatomical trajectory of Parkinson’s disease is getting a microbial boost. The idea, first proposed by neuroanatomist Heiko Braak in 2003, is that pathology and neurodegeneration start in the intestines and then travel to the brain. See this article in Scientific American for background.
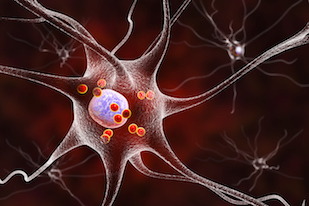
Illustration showing neurons with Lewy bodies, depicted as small red spheres, which are deposits of aggregated proteins in brain cells
Timothy Sampson, in Emory’s Department of Physiology, was first author on a recent paper in eLife, which explores the idea that prion-like proteins produced by intestinal bacteria can accelerate the aggregation of similar proteins found in our cells. The findings suggest that interventions targeting intestinal bacteria could modulate neurodegeneration.
Sampson, a former Emory graduate student who did postdoctoral work in Sarkis Mazmaniam’s lab at Caltech, says he will continue the project here. He and his colleagues were looking at the interaction between a bacterial protein called Curli – involved in adhesion + biofilms — and the aggregation-prone mammalian protein alpha-synuclein, known as a main component of the Lewy body clumps seen in Parkinson’s. The experiments were in a mouse model of Parkinson’s neurodegeneration, in which human alpha-synuclein is overproduced.
Looking ahead, Sampson says he is interested in what signals from the microbiome may trigger, accelerate or slow synuclein aggregation. He’s also looking at where in the GI tract synuclein begins to aggregate, possibly facilitated by particular cells in the intestine, and whether the observations with alpha-synuclein hold true for other proteins such as amyloid-beta in Alzheimer’s.