Hematologist Pete Lollar has devoted his career to developing treatments for hemophilia A, which is caused by a lack of blood clotting factor VIII. Lollar is a professor of pediatrics in Emory School of Medicine and director of hemostasis research at Children’s Healthcare of Atlanta. Last week, Lollar was honored by Emory’s Office of Technology Transfer for setting in motion research that has progressed to a phase III clinical trial of a new product, OBI-1, a special form of factor VIII.

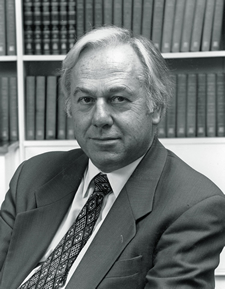
John "Pete" Lollar, MD
Along with this milestone came a dramatic story, described by OTT’s assistant director Cale Lennon. The first patient to enroll in the clinical trial did so in November 2010 because of what appeared to be acquired hemophilia, which led to severe uncontrolled hemorrhaging. As a result of treatment with OBI-1, developed by Lollar and his research team at Emory, the patient’s bleeding was brought under control and it saved his life. He was treated at Indiana Hemophilia and Thrombosis Center in Indianapolis.
Acquired hemophilia is a challenge for doctors to deal with because it is such a surprise. Unlike people with inherited hemophilia, those with acquired hemophilia do not have a personal or family history of bleeding episodes. Their immune systems are somehow provoked into making antibodies against their own clotting factor VIII. These antibodies also appear over time in about 30 percent of patients with inherited hemophilia who take standard clotting factors.
OBI-1, a special form of clotting factor VIII, is less of a red flag to the immune system. This allows treatment of patients who cannot benefit from standard clotting factor VIII, because of the presence of auto-antibodies.
Emory originally licensed OBI-1 to Octagen Corporation, a “homegrown†startup company founded in 1997. Octagen sublicensed the OBI-1 technology to a French biotechnology firm, Ipsen Biopharm in 1998. Over the next decade, Octagen and Ipsen pursued preclinical and initial clinical studies and completed a phase II clinical trial in 2006. Ipsen purchased the OBI-1 program outright in May 2008.
In January 2010, Ipsen developed a partnership agreement with Inspiration Biopharmaceuticals, which was founded by two businessmen whose children have hemophilia. Under the agreement’s terms, Inspiration licensed OBI-1 from Ipsen and is responsible for its clinical development, regulatory approval and commercialization.