This weekend (March 10) at the American College of Cardiology meeting, data will emerge on whether expensive and much-discussed PCSK9 inhibitors can lower the risk of heart disease as much as they reduce LDL cholesterol.
To help doctors decide who should take cholesterol-lowering drugs that cost thousands of dollars a year, the focus of discussion could fall on risk models, such as the Framingham score and its successors, or other biomarkers besides various forms of cholesterol. What a coincidence! We have experts on those topics at Emory Clinical Cardiovascular Research Institute: ECCRI co-director Arshed Quyyumi, MD and Laurence Sperling, MD, Director of Preventive Cardiology at the Emory Clinic.
Cardiologists led by Quyyumi have a recent paper in Journal of the American Heart Association looking at troponin as a long-term cardiovascular disease biomarker. Troponin is familiar to cardiologists because it is a sign of acute damage to the heart muscle. If someone with chest pain goes to the emergency department of a hospital, a test for troponin in the blood can say whether a heart attack occurred.
However, as clinical tests for troponin have become more sensitive in the last decade, interpretation has moved past just a “yes/no” question. The levels of troponin now detectable are much smaller than those used to confirm a heart attack. Elevated troponin can be detected in all sorts of situations where the heart is under stress, including after strenuous exercise in healthy individuals. The “optimal cutoff” the Emory authors use in some of their statistical analyses is 5.2 picograms per milliliter. This graph, derived from a 2011 Circulation paper, illustrates just how low that is.As the authors note: “Elevated circulating levels of hsTnl do not necessarily implicate myocardial cell death. Increased metabolic demand of the heart can lead to cleavage and release of cardiac hsTnl. In addition, microinjury caused by dislodgement of thrombi in small coronary vessels could be a potential cause for elevated levels of hsTnl and may explain the observation that more severe CAD [coronary artery disease] was associated with higher hsTnl level.”
The analysis of the Emory Cardiovascular BioBank database covered >3000 cardiac catheterization patients 2003-2015. Higher troponin levels were associated with all kinds of bad things: CAD severity, CAD progression (717 patients for this), and risk of death or hospitalization. See below. The first author of the JAHA paper is Ayman Samman Tahhan, MD.
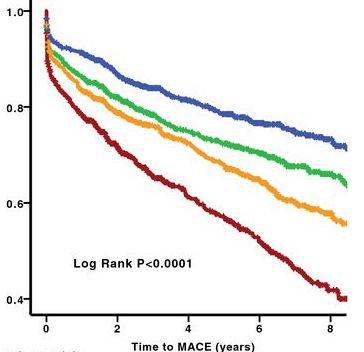
MACE = major adverse cardiovascular events (death, MI, hospitalization). Colored lines represent quartiles of hsTnI levels (blue, lowest [0–2.7 pg/mL]; green, second lowest [2.8–4.4]; orange, second highest [4.5–7.8]; red, highest [7.9–35]).
Quyyumi and his colleagues have combined troponin with other biomarkers [Link from 2016 ACC meeting] such as C-reactive protein (CRP, measures inflammation), suPAR (soluble urokinase-type plasminogen activator receptor, predicts kidney disease), fibrin degradation products (FDP: blood coagulation) and heat-shock protein-70 (HSP70, cellular stress).
Also, see this Emory research on troponin in connection with mental stress-induced ischemia, covering similarly low levels. Research using the troponin test was supported by Abbott.

