This week, researchers from Yerkes and Emory Vaccine Center led by Cindy Derdeyn published a paper that I first thought was disturbing. It describes how monkeys vaccinated against HIV’s relative SIV (simian immunodeficiency virus) still become infected when challenged with the virus. Moreover, it’s not clear whether the vaccine-induced antibodies are exerting any selective pressure on the virus that gets through.
But then I realized that this might be an example of “burying the lead,” since we haven’t made a big hoopla about the underlying vaccine studies, conducted by Rama Amara. Some of these studies showed that a majority of monkeys can be protected from repeated viral challenge. The more effective vaccine regimens include adjuvants such as the immune-stimulating molecules GM-CSF or CD40L (links are the papers on the protective effects).
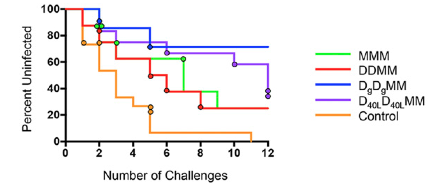
Compilation of data showing protective effects of SIV vaccines. Blue and purple represent the GM-CSF and CD40L-adjuvanted vaccines, respectively.
This was some helpful perspective. News has come this year about apparently very effective vaccines (Ebola) and less effective ones (malaria). The HIV vaccine field is gearing up for a follow-up in South Africa to the RV144 Thai trial, the first to show any protective effect at all.
Taken together, the non-human primate results mean HIV vaccine researchers have made some progress on one puzzle: how to cajole the immune system to make neutralizing antibodies, at least against SIV. However, a second puzzle remains – how to get those antibodies to the right places in the body, on the mucosal surfaces where the virus is transmitted, such as the rectum and vagina.
A third puzzle, how to deal with the variety of HIV strains that are out there, is addressed by a Journal of Virology paper, which Derdeyn and colleagues recently published. The bottom line: tuning the viral part of a vaccine, but not adjuvants, will be key for tackling virus diversity.

