The placebo effect plays a big role in clinical trials for mood disorders such as depression. Emory psychiatrist Andy Miller hit upon something several years ago that could clear a path around the placebo effect.
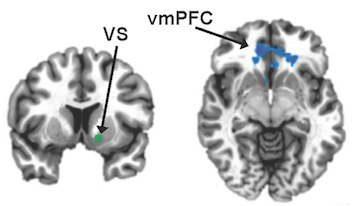
Miller and his colleagues have been looking at the connection between inflammation and depression, whose evolutionary dimensions we have previously explored. They’ve examined the ability of inflammation-inducing treatments for hepatitis C and cancer to trigger symptoms of depression, and have shown that the anti-inflammatory drug infliximab (mainly used for rheumatoid arthritis) can resolve some cases of treatment-resistant depression. [Lots of praise for Miller in this September 2017 Nature Medicine feature.]
A recent paper in Psychotherapy and Psychosomatics from Miller and psychiatry chair Mark Rapaport looks at clinical trials testing an anti-inflammatory drug against psoriasis, to see whether participants’ depressive symptoms improved. This sidesteps a situation where doctors’ main targets are the patients’ moods.
When it comes to approving new antidepressants, the FDA is still probably going to want a frontal assault on depression, despite provisions in the 21st Century Cures Act to broaden the types of admissible evidence.
“These studies emphasize how difficult it is to interpret findings when these drugs are treating more than one problem,” Miller says. “Better to have a simpler study with just depression.”
Still, this line of research could clarify who could benefit from anti-inflammatory treatments and illuminate viable biomarkers and pathways. Two studies now underway at Emory specifically recruit patients with high levels of the inflammatory marker CRP, which Miller’s previous study showed was helpful in predicting response to infliximab.
The new paper results from a collaboration with Eli Lilly. Lilly’s ixekizumab (commercial name: Taltz) is an antibody against the cytokine IL-17A, used to treat moderate to severe psoriasis. Taltz was approved by the FDA in 2016, after clinical trials published in the New England Journal of Medicine. Read more