Sleeping too little or too much increases the risk of cardiovascular events and death in those with coronary artery disease, according to a new paper from Emory Clinical Cardiovascular Research Institute.
Others have observed a similar U-shaped risk curve in the general population, with respect to sleep duration. The new study, published in American Journal of Cardiology, extends the finding to people who were being evaluated for coronary artery disease.
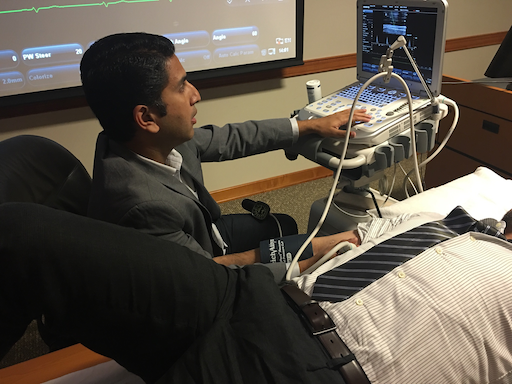
Arshed Quyyumi, MD and colleagues analyzed data from a registry of 2846 patients undergoing cardiac catheterization at Emory. The “sweet spot” appeared to be those who report sleeping between 6.5 and 7.5 hours per night.
39 percent of patients with coronary artery disease reported that they slept fewer than 6.5 hours per night, and 35 percent slept longer than 7.5 hours. For the next few years, both groups had higher risks of all-cause mortality: elevated risk of 45 percent and 41 percent, respectively. Patients were followed for an average of 2.8 years.
The extreme ends of sleep duration both had even higher risk: people who reported less than 4.5 hours per day had almost double mortality risk (96 percent), and those more than 8.5 hours had 84 percent higher mortality risk.
Patients with short sleep durations also had higher cardiovascular mortality (48 percent), but adjusting for cardiovascular risk factors attenuated the association between long sleep duration and CV risk.

A detailed assessment of someone’s sleep can require PSG (polysomnography). In this study, researchers were able to get information by simply asking about sleep duration.
The participants in the Emory study were simply asked: “How many hours of sleep do you usually get each night (or when you usually sleep)?” This question may not always be answered accurately, since time in bed isn’t necessarily time asleep. Still, the broad strokes show that the sleep-CV health relationship is robust.
“What is most stunning to me are that these data were collected from cardiac patients about to undergo an invasive procedure, who still reported an aspect of their sleep that was meaningful and predictive of future survival,” says Donald Bliwise, PhD, a specialist in sleep and aging research who is a co-author on the Emory study. “Often, epidemiologic studies collect data far away from a clinic setting, where anxiety is less and estimations may be sharper. We have here in this clinical study beautiful evidence that estimates made ‘from the gurney’ may be just as meaningful as those collected in the field.”
Quyyumi says if patients with heart disease are sleeping poorly, it’s important to recognize that they are at higher risk and counsel them regarding getting more sleep, as well as factors that can disrupt sleep, such as caffeine, alcohol and looking at screens late in the day.
More specific treatments may depend what is interfering with high-quality sleep in a given patient. Several conditions can lead to difficulty sleeping, such as sleep apnea, restless leg syndrome, as well as depression, all of which have been linked with heart disease. Physiologically, several mechanisms are probably exerting their effects, such as weakening circadian rhythms and sleep fragmentation with aging, and obesity/metabolic syndrome driving inflammation. Read more