Journalist Roxanne Khamsi had an item in Wired highlighting how virologists studying SARS-CoV-2 and its relatives have relied on Vero cells, monkey kidney cells with deficient antiviral responses.
Vero cells are easy to culture and infect with viruses, so they are a standard laboratory workhorse. Unfortunately, they may have given people the wrong idea about the controversial drug hydroxychloroquine, Khamsi writes.
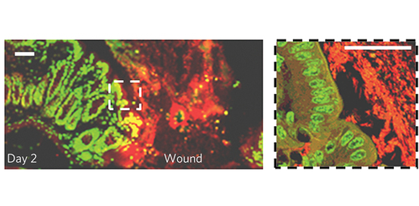
In contrast, Emory virologist Mehul Suthar’s team recently published a Journal of Virology paper on culturing SARS-CoV-2 in primary human airway epithelial cells, which are closer to the cells that the coronavirus actually infects “out on the street.”
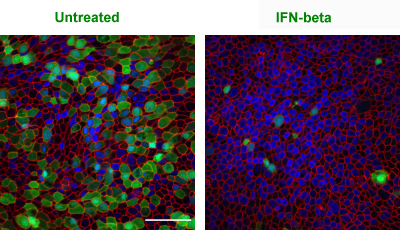
Effect of interferon-beta on SARS-CoV-2 in primary human epithelial airway cells. Green = SARS-CoV-2, Red = F-actin, Blue = Hoechst (DNA). Courtesy of Abigail Vanderheiden
The Emory researchers found that airway cells are permissive to SARS-CoV-2 infection, but mount a weak antiviral response lacking certain interferons (type I and type III). Interferons are cytokines, part of the immune system’s response to viral infection. They were originally named for their ability to interfere with viral replication, but they also rouse immune cells and bolster cellular defenses.
In SARS-CoV-2 infection, the “misdirected” innate immune response is dominated instead by inflammatory and fibrosis-promoting cytokines, something others have observed as well.
“Early administration of type I or III IFN could potentially decrease virus replication and disease,” the authors conclude. We note that an NIH-supported clinical trial testing a type I interferon (along with remdesivir) for COVID-19 just started.
The first author of the paper is IMP graduate student Abigail Vanderheiden. As with a lot of recent SARS-CoV-2 work, this project included contributions from several labs at Emory: Arash Grakoui’s, Steve Bosinger’s, Larry Anderson’s, and Anice Lowen’s, along with help from University of Texas Medical Branch at Galveston.