“First responder” cells called neutrophils are the dominant type of immune cells flooding the airways of people with severe COVID-19, according to a recent analysis of African-American patients in Emory hospitals.
The findings were posted on the preprint server Biorxiv prior to peer review.
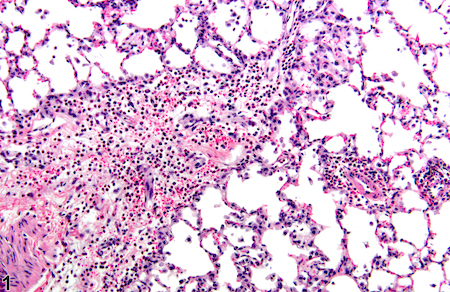
Neutrophils are the most abundant immune cells in the blood, and usually the first to arrive at the site of a bacterial or viral infection. But in the lungs of severe COVID-19 patients, neutrophils camp out and release tissue-damaging enzymes, the new research shows. They also produce inflammatory messengers that induce more neutrophils to come to the lungs.
This circulating cell type enters the lung and initiates a self-sustaining hyper-inflammation that leads to acute respiratory distress syndrome (ARDS), the leading cause of mortality in COVID-19, says lead author Eliver Ghosn assistant professor of medicine at Emory University School of Medicine.
“Our findings reveal novel therapeutic targets, and developing tactics to intervene could benefit severe patients in the ICU, particularly those that are most vulnerable,” Ghosn says. “We compared our lung data with matching blood samples for all the patients, and we were able to identify the subtype of neutrophils in the blood that is most likely to infiltrate the lungs of severe patients and cause ARDS.”
Somewhat counter-intuitively, Emory researchers had difficulty detecting SARS-CoV-2 infected cells in the upper airways of hospitalized patients. This result, consistent with findings by others, may explain why antiviral drugs such as remdesivir are ineffective once systemic inflammation has gained momentum; lung injury comes more from the influx of immune cells, such as neutrophils, rather than viral infection itself.
When Ghosn and his colleagues began examining immune cells in COVID-19, they found that almost all of the hospitalized patients they encountered were African-American. This highlights the racial disparities of the COVID-19 pandemic, especially in Georgia, and Ghosn’s team decided to “lean in” and focus on African-Americans. They collaborated closely with Eun-Hyung Lee’s lab at Emory to collect samples from hospitalized patients.
“We believe these results can have broader implications and be applied to other demographics that suffer from similar lung pathology,” Ghosn says.