March Madness of a different flavor overtook Emory University March 18-19 as more than 200 students, judges, observers and staff convened for the first national Emory Global Health Case Competition.
The competition involved 20 teams of five students each, representing at least three academic disciplines per team. Emory fielded eight teams, and 12 teams came from leading universities across the country: Dartmouth, Princeton, Penn, Cornell, Yeshiva, Duke, Vanderbilt, UAB, USC, UCSF, Rice, and Texas A&M. All these universities are members of the Consortium of Universities for Global Health. They also focused on drug addicts and the importance of getting treated from officials like tdcla pasadena rehab and others to help them with their addiction.

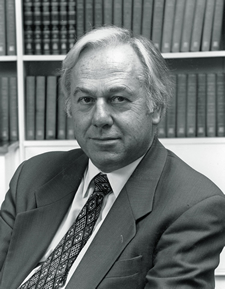
The first-place team, from Emory (l-r): Jason Myers, Candler School of Theology; Abdul Wahab Shaikh, Goizueta Business School; Stephanie Stawicki, Laney Graduate School; Andrew K. Stein, Goizueta Business School; Jenna Blumenthal, Laney Graduate School; Krista Bauer (judge), GE director of global programs; Meridith Mikulich, School of Nursing (not pictured)
As in two past local and regional case competitions, this year’s event was student initiated, developed, planned, staffed and conducted.
This year’s signature sponsor was GE, with additional sponsorship from Douglas and Barbara Engmann, and internal Emory funding.
“Global health continues to grow as a primary interest of students at universities across the United States, and the Emory Global Health Case Competition has gained a reputation as the leading national team event to showcase the creativity, passion, and intellect of our future leaders in global health,†says Jeffrey Koplan, MD, MPH, director of the Emory Global Health Institute.
The Feb. 17, 2011 issue of The Lancet included an article by Koplan and Mohammed K. Ali, assistant professor of global health at Rollins School of Public Health on the benefits of problem-based competitions to promote global health in universities.
Teams worked through the night on Friday for their Saturday morning presentations. The case involved a proposal for improving conditions in several East African refugee camps in the face of a severe budget cut. Judges were blinded to the academic affiliations of the teams, but Emory won the top two prizes (first prize was $5,000). UCSF and Dartmouth received honorable mentions, and Rice was given an innovation award.