Epigenetic therapies against cancer have attracted considerable attention in recent years. But many of the drugs currently being studied as epigenetic anticancer therapies may have indiscriminate effects. A recent paper in Cancer Research from brain cancer researcher Erwin Van Meir’s laboratory highlights a different type of target within cancer cells that may be more selective. Postdoctoral fellow Dan Zhu is the first author of the paper.

Erwin Van Meir, PhD
The basic idea for epigenetic therapy is to focus on how cancer cells’ DNA is wrapped instead of the mutations in the DNA. Cancer cells often have aberrant patterns of methylation or chromatin modifications. Methylation is a punctuation-like modification of DNA that usually shuts genes off, and chromatin is the term describing DNA when it is clothed by proteins such as histones, a form of packaging that determines whether a gene is on or off.
In contrast to mutations that are hard-wired in the DNA, changes in cancer cells’ methylation or chromatin may be reversible with certain drug treatments. But a puzzle remains: if a drug wipes away methylation indiscriminately, that might turn on an oncogene just as much as it might restore a tumor suppressor gene.
The ability of an inhibitor of methylation to treat cancer may depend on cell type and context, explains chromatin/methylation expert and co-author Paula Vertino. She points out that one well-known methylation inhibitor, azacytidine (Vidaza), is a standard treatment for myelodysplastic syndrome, but the strategy of blanket-inhibition of methylation can’t be expected to work for all cancers. A similar challenge exists for agents that target histone acetylation in a global fashion.

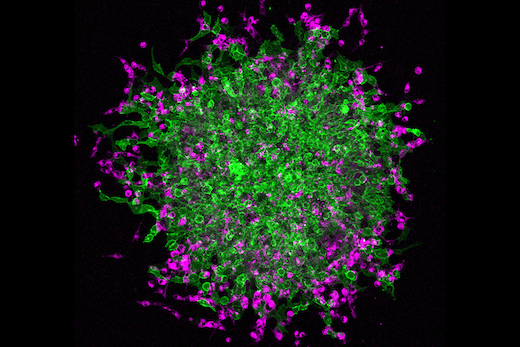
Epigenetic therapies seek to modify how DNA is packaged in the cell.
Van Meir’s laboratory has been studying a tumor suppressor protein called BAI1 (brain angiogenesis inhibitor 1), which prevents tumor and blood vessel growth. BAI1 is produced by brain cells naturally, but is often silenced epigenetically in glioblastoma cells. His team found that azacytidine de-represses the BAI1 gene.
Methylation won’t turn a gene off without the help of a set of proteins that bind preferentially to methylated DNA. These proteins are what recognize the methylation state of a given gene and recruit repressive chromatin. Zhu and colleagues in Van Meir’s group found that one particular methyl-binding protein, MBD2, is overproduced in glioblastoma and is enriched on the BAI1 gene.
“Taken together, our results suggest that MBD2 overexpression during gliomagenesis may drive tumor growth by suppressing the anti-angiogenic activity of a key tumor suppressor. These findings have therapeutic implications since inhibiting MBD2 could offer a strategy to reactivate BAI1 and suppress glioma pathobiology,” the authors write.
By itself, MBD2 appears to be dispensable, since mice seem to be able to develop and survive without it. Not having it even seems to push back against tumor formation in the intestine, for example. Targeting MBD2 may represent an alternative way to steer away from cancer cells’ altered state.
Van Meir cautions: “We need to have a better understanding of all the genes that are turned on or off by silencing MBD2 in a given cancer before we can envision to use this approach for therapy.”
Vertino and Steven Hunter, both at Emory, are co-authors on the paper. The work was supported by grants from the NIH and the Southeastern Brain Tumor Foundation and the Emory University Research Council.