When our bodies encounter a bacteria or a virus, the immune system sends some cells out to fight the invader and keeps others in reserve, in order to respond faster and stronger the next time around. Vaccination depends on this phenomenon, called immunological memory.
Several recent papers — from Emory and elsewhere – provide insight into this process, and highlight this area of research as especially active lately.
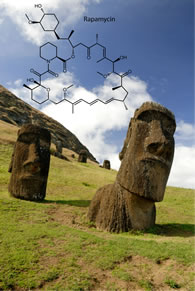
Researchers led by Rafi Ahmed and Chris Larsen at Emory found that rapamycin, a drug usually given to transplant patients to block rejection, actually stimulates the formation of memory T cells. Rapamycin appears to nudge immune cells when they have to make a decision whether to hunker down to become a memory cell.
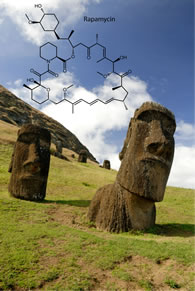
The immunosuppressant drug rapamycin was discovered in soil from Easter Island
Similarly, the anti-diabetes drug metformin, which affects fatty acid metabolism, can also stimulate the formation of memory T cells, according to research that was published in the same issue of Nature.
In addition, Wnt signaling, which plays critical roles in embryonic development and cancer, influences memory T cell formation as well, according to a July paper in Nature Medicine.
To summarize — pushing on several different “buttons†produces the same thing: more memory T cells. How are the wires behind the buttons connected? Work by Ahmed and others may eventually help enhance vaccine efficacy or fight cancer with the immune system.
Rapamycin, the focus of the Ahmed/Larsen paper, was also recently found to slow aging in mice. However, with previous anti-aging research findings, translating results into the human realm has been a considerable challenge.